Vitamin D: Deficiency Symptoms, Health Benefits, Optimal Sources, And Side Effects
Authored by Mecura Wang and medically reviewed by Dr. Beverly Timerding via The Epoch Times,
Vitamin D, or the “sunshine vitamin,” is considered both a fat-soluble vitamin and a hormone because it can be obtained nutritionally, and our skin can synthesize it through sunlight exposure. It is integral to various bodily functions.
Primarily recognized for enhancing calcium absorption, vitamin D plays a role in maintaining bone and dental health, supporting the immune system, regulating cell growth, influencing mood, and preventing conditions such as multiple sclerosis.

What Are the Signs and Symptoms of Vitamin D Deficiency?
Vitamin D deficiency is the most prevalent nutritional deficiency, affecting people of all ages globally. In the United States, nearly one-quarter of individuals have insufficient or deficient vitamin D blood levels, which can impact bone and overall health. Approximately 50 percent of children between ages 1 and 5 and 70 percent aged 6 to 11 experience vitamin D deficiency.
Vitamin D deficiency often arises due to insufficient sunlight exposure, inadequate dietary intake, and the skin’s inability to produce it. Also, natural foods typically do not provide enough vitamin D to prevent deficiency, making sunlight exposure a crucial factor.
Most people with vitamin D deficiency experience no symptoms. For others, common symptoms may include:
- Fatigue: Vitamin D deficiency has been linked to fatigue in uncontrolled trials, and treatment with the vitamin has been shown to improve the condition in blinded, randomized, placebo-controlled trials. Individuals with persistent and severe vitamin D deficiency may encounter symptoms linked to secondary hyperparathyroidism, including fatigue. Secondary hyperparathyroidism is when the parathyroid excretes too much hormone due to low calcium levels.
- Bone and muscle pain: A mild but prolonged vitamin D deficiency can result in chronic hypocalcemia (low calcium) and hyperparathyroidism, with symptoms such as bone pain and muscle aches.
- Muscle weakness and cramps (spasms): Increased levels of vitamin D in the bloodstream have been linked to enhanced muscle strength, physical activity, and the capability to ascend stairs, while lower concentrations are associated with a higher risk of falls among older people. Muscle spasms, particularly in infants, can be an early indication of rickets due to low blood calcium levels resulting from severe vitamin D deficiency.
- Mood changes: According to a systematic review, about a third of the studies indicated inadequate vitamin D levels were associated with depression. Others suggested supplementing with it was helpful if combined with exercise or along with other nutritional supplements.
- Bone loss: Vitamin D deficiency can cause bone loss as it impairs calcium absorption, leading to decreased calcium levels in the blood. Specifically, insufficient vitamin D limits the body’s ability to absorb only 10 percent to 15 percent of dietary calcium, whereas with normal vitamin reserves, absorption typically ranges from 30 percent to 40 percent.
Other symptoms and signs of deficiency may include:
- Heightened pain sensitivity
- A tingling sensation in the hands or feet
- A waddling gait from weakened hip or leg muscles
- Bone fractures
- Bowed legs (severe deficiency)
- Knock-knees
- Poor sleep
- Hair loss
- Increased susceptibility to illness
Complications
The complications of vitamin D deficiency are:
- Rickets: Rickets affects children’s bones, causing them to become soft and weak, potentially leading to deformities. Symptoms and signs include bone pain, reluctance to walk, skeletal deformities such as bowed legs, thickening of joints, dental issues, delayed growth, and fragile bones prone to fractures in severe cases.
- Osteoporosis: Vitamin D deficiency can result in secondary hyperparathyroidism, leading to bone loss, osteoporosis, fractures, mineralization defects, and long-term risks of osteomalacia. Osteoporosis may cause intense back discomfort, diminished stature, or deformities in the spine, such as a bent or hunched posture.
- Osteomalacia: This is similar to rickets but can happen at any age. Characterized by bone softening, osteomalacia is primarily linked to vitamin D issues negatively affecting calcium absorption. Its symptoms and signs include bone fractures, muscle weakness, and widespread bone pain, particularly in the hips.
What Are the Health Benefits of Vitamin D?
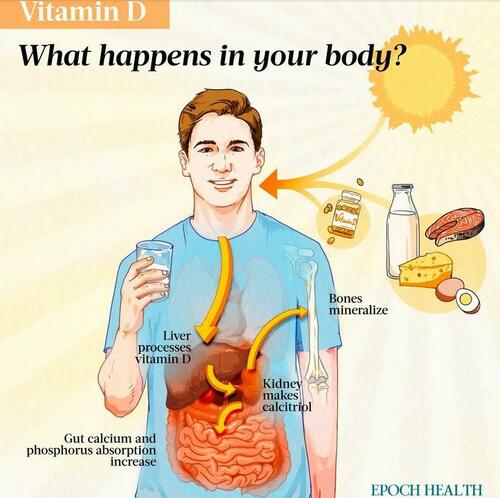
When you eat food or supplements containing vitamin D, your body undergoes two processes to activate it. First, in the liver, vitamin D is converted to calcidiol (25-hydroxyvitamin D). After that, the kidneys further transform it into calcitriol (1,25-dihydroxyvitamin D).
Calcitriol encourages the absorption of calcium and phosphorus in the small intestine. It also works with parathyroid hormone to enhance calcium transport, which is essential for maintaining proper calcium and phosphorus levels.
Vitamin D plays a crucial role in calcium absorption, essential for strong bones and teeth. It also supports muscle and nerve function, facilitating movement and communication within the body. In addition, vitamin D is vital for the immune system, as it helps defend against infections.
- Bone health: Vitamin D helps with the absorption of calcium and phosphorus, promoting bone mineralization and bone mineral density. A meta-analysis of 12 studies involving over 42,000 individuals aged 65 and above discovered that the prevention of nonvertebral fractures with vitamin D is dependent on the dosage. A higher dose of about 500 to 800 international units (IU) resulted in a reduction of hip fractures by 18 percent and nonvertebral fractures by 20 percent for people aged 65 years or older. However, in another study involving over 25,000 generally healthy midlife and older adults, supplementing with vitamin D3 did not lead to a significantly lower risk of fractures compared to a placebo. Of note, though, patients in this study had no controlled calcium supplementation.
- Muscle and nerve function: Vitamin D may contribute to increased muscle strength by preserving muscle fibers, potentially reducing the risk of falls, a prevalent issue associated with significant disability and mortality in older individuals. Research also suggests that vitamin D plays a vital role in essential neurological functions such as cell growth, development, nerve support, protection, signal transmission, and adaptability.
- Immune system support: Vitamin D contributes to a healthy immune system. The vitamin D receptor is present in immune cells, allowing vitamin D to act locally in the immune system. The vitamin can influence both the innate and adaptive immune responses and its deficiency is linked to higher autoimmunity risk and increased vulnerability to infections. Moreover, vitamin D exhibits strong anti-inflammatory effects.
Other health benefits of vitamin D include:
- Pregnancy support: Vitamin D supplementation during pregnancy has also been associated with a reduction in the risks of small-for-gestational-age babies, preeclampsia, preterm birth, and gestational diabetes.
- Mood regulation
- Insulin level regulation: Vitamin D has been shown to lower blood glucose levels and enhance insulin sensitivity in people with diabetes.
- Weight loss: Vitamin D plays a role in preventing the formation of fat cells by influencing specific molecules, such as vitamin D receptors.
- Dental health: Research highlights a link between alveolar bone density, osteoporosis, tooth loss, and periodontal disease risk. Several reports suggest a significant connection between periodontal health and vitamin D intake.
Vitamin D Prevents Certain Conditions
In addition to the aforementioned bone-related and mental medical conditions, an adequate level of vitamin D can potentially prevent or lower the risk of certain diseases, including:
- Certain types of cancer: Animal and lab studies suggest that vitamin D may inhibit tumor development and slow the growth of existing tumors in various organs, including the breast, ovary, colon, prostate, and brain. Human epidemiological studies demonstrate that higher serum levels of vitamin D are linked to significantly slower progression of certain cancers, particularly colorectal cancer. The anti-cancer effects of vitamin D may also extend indirectly through its anti-inflammatory properties.
- Heart disease: Maintaining optimal vitamin D levels may have potential cardiovascular health benefits, according to one recent study. Both deficiency and insufficiency of vitamin D were linked to an increased risk of cardiovascular diseases (CVD), including stroke, heart disease, heart attack, and heart failure. However, excess vitamin D was not associated with increased CVD risk.
- Immune-related diseases: Sufficient vitamin D levels may help prevent or treat immune-related diseases.
- Asthma: A meta-analysis discovered that taking vitamin D supplements helped adults with mild-to-moderate asthma who were also deficient in vitamin D to reduce their asthma exacerbations by 30 percent. However, this benefit was not observed in individuals with higher baseline vitamin D levels.
- Atherosclerosis: Vitamin D’s anti-inflammatory properties appear promising in lessening atherosclerosis, as insufficient levels lead to increased production of pro-inflammatory markers, disrupting the balance in the inflammatory response. In atherosclerosis, vitamin D suppresses the production of pro-inflammatory cytokines, which play a significant role in the development of the disease.
- Type 2 diabetes: One study suggested a higher prevalence of vitamin D deficiency in patients with Type 2 diabetes. Insulin resistance decreases with the supplementation of vitamin D.
- Autoimmune diseases: Extensive research indicates a potential connection between vitamin D deficiency and the development of autoimmune diseases. Vitamin D deficiency has been noted in conditions such as rheumatoid arthritis, with an inverse relationship to disease activity, suggesting a role in the disease’s pathogenesis. Similar observations exist for systemic lupus erythematosus (SLE), Sjögren’s syndrome, ankylosing spondylitis, psoriatic arthritis, and idiopathic inflammatory myopathies. Research also indicates there is a lower risk of developing multiple sclerosis in individuals with higher levels of vitamin D.
- Cognitive decline: Research has consistently established a connection between cognitive impairment, dementia, and a lack of vitamin D.
- Mortality: As per a meta-analysis of 18 studies involving 57,311 subjects, daily intake of vitamin D supplements was associated with a reduction in all-cause mortality rates.
What Are the Types of Vitamin D?
Vitamin D is not a single chemical but a group of compounds. The two major types of vitamin D are D2 and D3. Vitamin D2 and D3, collectively known as vitamin D, share nearly identical functions, yet neither becomes active until the body performs its transformative process.
1. Vitamin D2 (Ergocalciferol)
Vitamin D2 comes from plants and fungi and is created when ergosterol is exposed to radiation. It is found in some plant-based foods and used in vitamin D supplements.
2. Vitamin D3 (Cholecalciferol)
The body naturally produces a form of vitamin D from a widespread cholesterol variant called 7-dehydrocholesterol, mainly through exposure to sunlight. UVB energy from sunlight plays a crucial role in converting this precursor into vitamin D3. It is also found in some animal-based foods, such as fatty fish, egg yolks, and liver.
Vitamin D3 is commonly available in animal-based supplements. It is often considered more effective than D2, possibly due to its stronger connection with the vitamin D binding protein. This increased affinity may result in slower clearance of vitamin D3, leading to longer-lasting concentrations of 25(OH)D in the blood compared to D2.
What Is the Recommended Amount of Vitamin D?
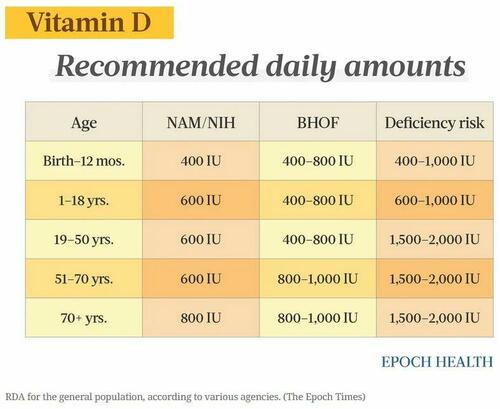
The required daily amount of vitamin D varies based on an individual’s age. The recommended dietary allowance (RDA) for vitamin D is designed to meet the daily requirements for maintaining healthy bones and normal calcium metabolism in individuals with minimal sun exposure.
The recommended daily intake of vitamin D can vary among different organizations, such as the National Academy of Medicine (NAM) (formerly known as the Institute of Medicine, or IOM), which is part of the National Academies of Sciences, Engineering, and Medicine (NASEM), the Bone Health & Osteoporosis Foundation (BHOF) (formerly known as National Osteoporosis Foundation, or NOF), and the Endocrine Society.
The NAM RDA guideline below is also recommended by the National Institutes of Health (NIH). NAM considers these intake amounts adequate to achieve a vitamin D blood level of 50 nanomoles per liter (nmol/L), which they believe is sufficient for most people. In addition, according to the Endocrine Society, ensuring a consistent elevation of the blood level of 25(OH)D above 75 nmol/L may necessitate a daily intake of at least 1,000 IU of vitamin D.
The following table compares the recommended daily vitamin D amounts by the NAM and NIH, BHOF, and the Endocrine Society.
What Types of Vitamin D Supplements Are Available?
Vitamin D supplements are available in three types: vitamin D2, vitamin D3, and calcidiol. However, calcidiol is considered a medication, and it may be prescribed for individuals with health conditions causing malabsorption, such as cystic fibrosis, celiac disease, or liver disease, which impairs the synthesis of calcidiol from typical vitamin D supplements.
Vitamin D2 vs. D3 Supplements
Vitamin D2 supplements are created by subjecting a plant sterol to ultraviolet energy, resulting in the production of vitamin D2. Vitamin D3 is usually generated through the irradiation of 7-dehydrocholesterol derived from lanolin obtained from sheep’s wool. Individuals who abstain from all animal-derived products can ask manufacturers about supplement sourcing and processing methods.
Ongoing debate surrounds the preference for vitamin D3 over D2 to increase blood levels. A meta-analysis suggests that D3 supplements tend to raise and maintain vitamin D levels more effectively than D2. Many experts favor vitamin D3 due to its natural production in the body and its presence in foods containing the vitamin.
One study involving 15,716 participants compared four treatment options for vitamin D deficiency, including vitamin D2 injection, vitamin D3 injection, a combination of vitamin D2 injection with a D2 tablet, and a combination of vitamin D3 injection with a D2 tablet. All treatments led to a significant increase in serum vitamin D within 12 weeks, with the vitamin D3 injection alone showing the highest increase. The findings suggest that using vitamin D3 in injectable form is the most effective option for restoring severe vitamin D deficiency, outperforming the injectable form of vitamin D2 and D2 tablets. However, the study did not address the effects of a vitamin D3 tablet/capsule, which is still generally better absorbed than oral vitamin D2.
Different Forms of Vitamin D Supplements
Vitamin D2 and D3 supplements can be obtained over the counter or by prescription in the United States. They come in various strengths, including 400, 800, 1,000, 2,000, 5,000, 10,000, and 50,000 IU, with the latter requiring a prescription.
For adults, the general recommendation is a daily supplement containing 800 IU. Older individuals may still experience vitamin D deficiency at this intake level, so they might need to increase the dosage per their doctor’s instructions. In addition, all infants and children are advised to take a vitamin D supplement containing 400 IU starting shortly after birth.
As vitamin D is fat-soluble, it is most effectively absorbed when consumed with a meal or snack containing some fat.
Vitamin D supplements are also available in various forms, including:
- Capsules/softgels
- Tablets
- Liquid drops
- Gummies
- Sprays
- Injections
What Are the Dietary Sources of Vitamin D?
Vitamin D is found naturally in a few foods, and most dietary intake in the United States comes from fortified foods supplemented with vitamin D.
Vitamin D2
- Many plant-based milks (e.g., soy, almond, and oat) and plant-based yogurts are fortified with vitamin D2. One cup of various soy, almond, and oat milk brands is fortified with 100 to 144 IU of vitamin D.
- Some mushrooms naturally contain vitamin D2, and certain commercially sold ones have higher levels of D2 because they are intentionally exposed to high amounts of ultraviolet light. Half a cup of raw, sliced white mushrooms exposed to UV light contains 366 IU of vitamin D.
- Vitamin D (both D2 and D3) is supplemented in various breakfast cereals. One serving of ready-to-eat cereal is fortified with 10 percent of the daily value (DV) for vitamin D (80 IU).
- Some orange juice brands, margarine, and other food items are fortified with vitamin D2.
Vitamin D3
Vitamin D3 is obtained from animal products, with oily fish, fish oils, eggs, and dairy serving as the best dietary sources. The amount of vitamin D in an animal’s tissues is influenced by its diet.
Most of the U.S. cow’s milk supply is fortified with approximately 120 IU of vitamin D3 per cup, and infant formula is fortified. However, foods derived from milk, such as cheese and ice cream, are typically not fortified. Rich sources of vitamin D3 include fatty fish such as trout, salmon, tuna, and mackerel, as well as fish liver oils. In addition to vitamin D3, animal-based foods often contain calcidiol, also known as 25(OH)D. Research suggests that calcidiol is around five times more effective than the parent vitamin in increasing serum 25(OH)D concentrations.
Examples of foods containing vitamin D3 include:
- Fish oil: 1 tablespoon of cod liver oil (1,360 IU per serving)
- Trout: 3 ounces of cooked farmed rainbow trout (645 IU per serving)
- Salmon: 3 ounces of cooked sockeye salmon (570 IU per serving)
- Sardines: Two drained sardines, canned in oil (46 IU per serving)
- Cow’s milk: 1 cup of 2 percent milk fortified with vitamin D (120 IU per serving)
What Are the Other Sources of Vitamin D?
Unfortunately, we can obtain vitamin D from only diet, sun exposure, and supplementation. The belief that tanning beds can provide sufficient vitamin D is just a myth because tanning bed bulbs mainly emit UVA light, while vitamin D synthesis requires UVB light. Hypervitaminosis D (excessive vitamin D levels in the body) is a potential risk in a small proportion of tanning beds with UVB light. It’s not known if this is due to less heating of the skin in some facilities. Also, catching sunlight in a sunny office or while driving in a car won’t contribute to obtaining vitamin D, either, because window glass completely blocks UVB ultraviolet light.
Sunlight consists of two types of ultraviolet radiation: UVA and UVB. Although UVB is essential for the skin’s vitamin D synthesis, it can cause sunburn and contribute to cell damage linked to cancer. UVA also damages the skin and accelerates aging. To safeguard against sun damage and skin cancer, limit exposure during peak hours (10 a.m. to 2 p.m.), wear protective clothing such as a wide-brimmed hat and long-sleeved garments, and use sunscreen with SPF 30 or higher when too much exposure is unavoidable, ensuring it’s broad-spectrum for UVA and UVB protection.
Given the appropriate conditions, exposing the arms and legs to sunlight for 10 to 15 minutes a few times weekly can produce almost all the necessary vitamin D.
In addition to the aforementioned factors, elements affecting how much vitamin D your body makes include smog and other types of air pollution, season, and cloud cover. For instance, people living north of the 37-degree-latitude line, the imaginary line connecting Richmond, Virginia, and San Francisco, cannot obtain sufficient UVB exposure during winter to produce adequate vitamin D.
What Is the Treatment for Vitamin D Deficiency?
Blood 25(OH)D levels (combined vitamin D2 and D3) are a good indicator of vitamin D stores in the body and show a strong connection with symptoms and signs of deficiency. Blood tests measuring vitamin D, calcium, and phosphate levels can confirm a deficiency.
High-Risk Populations
Certain disorders, hereditary conditions, and medications may impact vitamin D absorption or conversion of vitamin D to its active form, thus contributing to deficiency.
The following risk factors put someone at higher risk of deficiency:
- Limited outdoor activity: Older adults and those residing in institutions may not have easy access to the outdoors.
- Inflammatory bowel diseases
- Celiac disease
- Cystic fibrosis
- Surgery: People who undergo bariatric or gastric bypass surgery for weight loss and those with sections of the small intestine removed (resection) are at higher risk.
- Darker skin: Less vitamin D is produced during sun exposure in darker skin compared to lighter skin, as the melanin in darker skin blocks and absorbs sunlight before it can initiate vitamin D production.
- Excessive sunscreen use
- Malabsorption disorders
- Age: As people age, their skin’s 7-dehydrocholesterol levels (which play a crucial role in the synthesis of vitamin D) decrease, accompanied by changes in the skin. Older people are also more prone to spending extended periods indoors.
- Certain medical conditions: Some conditions can hinder the body’s ability to synthesize or absorb sufficient vitamin D.
- Lactose intolerance: Milk is usually fortified with vitamin D.
- Vegan or vegetarian diets
To address vitamin D deficiency, increasing consumption of vitamin D-rich foods is often insufficient, prompting doctors to recommend supplements. The available forms of vitamin D supplements include vitamins D2 and D3 and calcidiol. The prescribed dosage varies based on factors such as severity, age, weight, and pregnancy status. The following table contains the suggested average daily dosages. The levels of 25-hydroxyvitamin D, or 25(OH)D, in the blood are used to measure vitamin D status.
Read the rest here…
Tyler Durden
Sat, 03/16/2024 – 19:50
via ZeroHedge News https://ift.tt/Z37tMsV Tyler Durden