The Unexpected Battle Between Vaccines And The COVID Virus
Authored by Yuhong Dong via The Epoch Times (emphasis ours),
Since the unprecedented COVID-19 global pandemic that started in January 2020, humans have been in a constant battle with the SARS-CoV-2 virus.
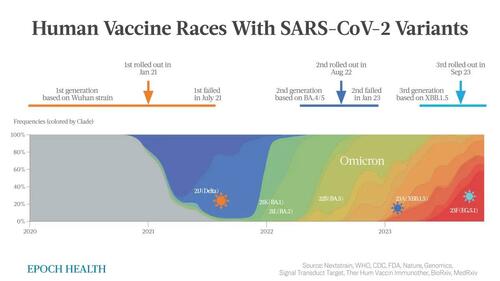
A series of vaccine versions have been developed and administered globally, beginning in January 2021 when an mRNA vaccine based on the original Wuhan strain was implemented. Subsequently, a bivalent mRNA vaccine was developed based on the Omicron offspring. Currently, the most updated version is based on XBB.1.5 and is ready to be injected into people’s arms.
Bivalent vaccines contain two different components. One component is to protect us against the original viral strain, while the other targets the most recent variants.
The vaccine is based on the gene code of a known virus, whereas the lead time for vaccine development normally takes an average of 10 years. Even with the current “green-light” policies for COVID-19 vaccines, it takes almost one year for the first generation to launch and a couple of months for the second and third generations.
However, due to the basic survival skills of SARS-CoV-2, the virus is always mutating in order to escape from a vaccine. Even before a vaccine is ready to launch, there are always a few mutants that have already found a way to escape from the antibodies induced by the sluggish vaccine, creating the next wave.
Regardless, the unprecedented speed of vaccine development won’t be able to compete with the speed of viral mutation, as the virus is always taking the lead and will be one step ahead of the vaccine.
This is why even the top scientists cannot predict how the virus will mutate and when the next wave will occur.
SARS-CoV-2 Variants
From 2020 to early 2021, a number of major SARS-CoV-2 variants have appeared: Alpha (B.1.1.7), Beta (B.1.351), Gamma(P.1), and Delta (B.1.617.2).
Not including those old variants, once Omicron (B.1.1.529) was first reported in South Africa in November 2021, it quickly evolved into a few sister lineages: BA.1, BA.2, BA.4, BA.5, XBB.1.5, EG.5, and HV.1, which each took the stage, one after the other within an interval of a couple of months.
- BA.1 and BA.2: first detected in February 2022.
- BA.4 and BA.5: first detected in May 2022.
- XBB.1.5 (Kraken): an offspring of two BA.2 sublineages first detected in October 2022.
- BA.2.86 (Pirola): first detected in 2023 and is currently being monitored.
- EG.5 (Eris): first detected in Feb 2023, peaked in October, and is now declining.
- HV.1: first detected in July 2023, has taken the lead in the United States at the end of October 2023.
The fierce battle between the virus and human technology has become a marathon. With each generation of vaccine development, who were the winners?
First Generation Vaccine: Delta Emerged, Creating Global Havoc
In January 2021, the original mRNA monovalent vaccines developed by Pfizer and Moderna and based on the old Wuhan strain were launched at a rocket-like speed.
In June 2021, when more than 50 percent of the U.S. population had received two doses of these vaccines, the stage was set for various mutants to take over, including the well-known alpha and delta variants.
A key mutation in spike protein called N501Y, which can escape from vaccine protection, was discovered in alpha. It was also found in two other major variants prevalent during that time and significantly increased in the rate at which it spread.
Shortly thereafter, Delta (B.1.617.2) emerged and presented even more enhanced transmissibility and vaccine escape ability with its intriguing spike protein double mutations of L452R and E484Q, refreshing the viral spreading and escaping records. It was designated as a “variant of concern” by the World Health Organization (WHO) on May 11, 2021.
These double mutations in the spike protein cause the vaccine-induced antibodies to significantly lose their ability to bind to delta, resulting in immunological evasion and causing major global havoc.
The increased binding affinity caused by delta makes it much easier to replicate in human cells. It was reported that patients infected with delta had a viral load 1000 times greater than patients with the original strain. It’s also been able to spread twice as fast as the original SARS-CoV-2 virus.
In July 2021, preliminary data from Israel showed that Pfizer’s vaccine efficacy was significantly reduced at five and six months after vaccination to 44 percent and 16 percent, respectively.
In a July 2021 outbreak in Massachusetts, 74 percent of breakthrough infections occurred in fully vaccinated persons, and the delta variant was detected in 90 percent of them.
The first round of the battle between the vaccine and the virus concluded with an overwhelming vaccine failure when the first generation of the COVID-19 mRNA vaccine met the unexpected delta variant.
Vaccine Versus Virus: The First Battle Round
Vaccine: Monovalent.
Result: The vaccine failed.
Time lapsed: Seven months from the first monovalent vaccine launched in January 2021 until the dominant delta wave in July 2021 in the United States.
Since then, a concern regarding the vaccine strategy of generating vaccine escape variants has been raised by scientists, including researchers from Michigan State University.
Second Generation Vaccine: XBB.1.5 Won
People continued to witness the declining effects of the original vaccine against delta, even after boosters were widely administered. The government continually stressed that the original vaccines had sufficient efficacy, one time after another.
Almost all of Omicron and its subvariants have developed specific mutations that have made them spread more quickly while evading our immune response. It has been clearly defined as an immune escape strain according to this Nature review.
A surprising virus, Omicron (B.1.1.529) surged more quickly than any previous strain and completely took over by April 2022. This emergence of hypermutated, increasingly transmissible Omicron variant significantly threatened the vaccine strategy.
It harbors multiple amino acid mutations in the spike (including Q498R and N501Y), which significantly enhance binding to the ACE2 receptor. It has also altered the cell entry pathway which further contributes to its ability to escape from vaccine protection.
In mid-2022, BA.4 and BA.5 lineages of Omicron were the dominant COVID-19 variants in the United States and were predicted to circulate in the second half of 2022.
Thus, Pfizer and Moderna quickly took the initiative to develop bivalent boosters based on the original strain from Wuhan and Omicron BA.4 and BA.5. They made it within another miraculously short time frame of just a few months.
On August 31, 2022, the FDA approved the bivalent booster shots of COVID-19 mRNA vaccines designed to target the Omicron subvariants BA.4 and BA.5, with Pfizer only providing the data on eight mice.
However, Omicron keeps quickly changing, splitting into even more diversified subgroups. Soon after the new bivalent vaccine was distributed, BA.4 and BA.5 became history.
A new variant XBB.1.5 began appearing in October 2022 and reached its peak in April 2023. It combines two descendent lineages (BA.2.10.1 and BA.2.75) of Omicron. The featured new spike protein mutation (F486P) leads to increased transmissibility and significant escape from the vaccine.
Not surprisingly, the antibody levels to XBB.1.5 in bivalent mRNA-boosted individuals declined significantly to pre-booster levels after only three months. The bivalent booster vaccine effectiveness against COVID-19-associated hospitalization declined to as low as 24 percent at six months post-vaccination, according to CDC data collected from September 2022 to April 2023.
The second round ended when the second generation bivalent mRNA vaccine encountered the XBB.1.5 starting in April 2023.
Vaccine Versus Virus: The Second Battle Round
Vaccine: Bivalent mRNA.
Result: The vaccine failed.
Time lapsed: Five months after the bivalent booster vaccine launched in September 2022 and was utilized until the U.S. dominant wave of XBB.1.5 in January 2023 emerged.
Third Generation Vaccine: Doomed to Fail
As of September 2023, the Pfizer-BioNTech and Moderna mRNA vaccines have been reformulated—for the third time—this time based on XBB.1.5, which is the great-grandchild of Omicron. This latest booster recommendation applies to all individuals, regardless of previous COVID-19 vaccination history.
However, one month before the 3.0 vaccine was approved, the dominant virus had already changed from XBB.1.5 to EG.5—the “Eris” variant, which spreads faster and has a stronger ability to escape from the XBB.1.5 vaccine.
Vaccine Versus Virus: The Third Battle Round
Vaccine: XBB.1.5 mRNA.
Result: Vaccine doomed to fail.
Time lapsed: Less than one month from the XBB.1.5 booster vaccine launch in October 2023 to the U.S. dominant wave of vaccine escape by EG.5 or other cousin variants in October 2023.
Omicron continues to change from XBB to JN, HK.3, EG.5, and HV.1—all belonging to the huge and diversified Omicron family.
EG.5, carrying an additional F456L mutation, is significantly more resistant to neutralization by the sera from vaccinated people. That means even the most recent version of the COVID-19 vaccine based on XBB.1.5 is going to lose its protection with EG.5. Since the risk of breakthrough infection remains high, the WHO listed EG.5 as a “variant of concern” in early August.
While HV.1 shares almost all spike mutations that EG.5 carries, it took on a surprising additional mutation (L452R) from a remote ancestor delta variant in 2011, which had normally disappeared in the omicron variant. HV.1 can further escape the XBB.1.5-based vaccine-induced immunity and is even more evasive than EG.5.
The same detour trick of HV.1 is also used by JN.1 coming on the scene in August 2023. It gains an additional L455S mutation, switching from the XBB sublineage to BA.2.86 (Pirola).
The HK.3 virus has played a novel trick. It has two mutations in the adjacent spike 455 and 456 positions (L455F and F456L), thus called a “FLip.” Together, this virus binds even more tightly to ACE2 and is taking off slowly in Brazil and Spain.
Both HK.3 (FLip) and JN.1 present even lower binding affinities, meaning the vaccine is even less effective than the current version, raising further concerns over vaccine strategy.
Despite the extraordinary speed of vaccine development against COVID-19 and the continued mass vaccination program, the never-ending emergence of new SARS-CoV-2 variants threatens to significantly overturn the vaccine’s intended effects.
This is a tiring battle between vaccines and the virus. The winners and losers are clear. The microscopic tricks utilized by the SARS-CoV-2 virus variants are far superior to the vaccines’ unproven technology.
Alerts have been raised and major concerns have been discussed by scientists as early as 2021 in top-ranked journals including The Lancet and Nature in addition to Nature Reviews, eBioMedicine (part of The Lancet Discovery Science), and other publications through 2023.
The common view is that the pressure exerted on viruses from repeated vaccination programs serves as a primary driver of the diversified variants of SARS-CoV-2.
If humans continue to develop vaccines based on these emerging new variants, there will continue to be repeated failures. How many more failures will it take to realize that all of these vaccine efforts have been in vain?
It is a time for rational deliberation to pause to reflect on finding the root cause of the viral infection.
We already have a dynamic shield of protection against serious viral attacks—our natural immunity. Only by facing our own innate immunity will the virus find its tricks useless.
Tyler Durden
Wed, 11/08/2023 – 20:20
via ZeroHedge News https://ift.tt/UiJNY0k Tyler Durden