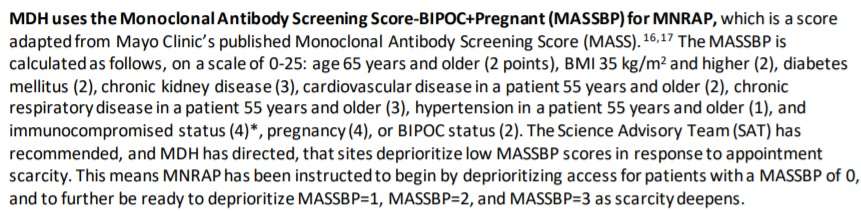
If you can’t read the image above (I’ve noticed a technical glitch with it), the text says:
MOH uses the Monoclonal Antibody Screening Score-BIPOC+Pregnant (MASSBP) for MNRAP, which is a score adapted from Mayo Clinic’s published Monoclonal Antibody Screening core (MASS). The MASSBP is calculated as follows, on a scale of 0-25: age 65 years and older (2 points), BMI 35 kg/m2 and higher (2), diabetes mellitus (2), chronic kidney disease (3), cardiovascular disease in a patient 55 years and older (2), chronic respiratory disease in a patient 55 years and older (3), hypertension in a patient 55 years and older (1), and immunocompromised status (4)*, pregnancy (4), or BIPOC status (2). The Science Advisory Team (SAT) has recommended, and MOH has directed, that sites de prioritize low MASSBP scores in response to appointment scarcity. This means MN RAP has been instructed to begin by deprioritizing access for patients with a MASSBP of 0, and to further be ready to deprioritize MAS5BP=l, MASSBP=2, and MASSBP=3 as scarcity deepens.
Note that people who lack “BIPOC status” (basically, non-Hispanic whites) would be “deprioritiz[ed]” precisely based on their race and ethnicity, not wealth, access to health care, being in a nursing home, or anything else. A rich non-white patient would be given priority over a poor white patient with precisely the same age and health conditions.
Here is the Department’s rationale:
The score was adapted after consultation with the University of Minnesota and Mayo Clinic to specifically examine the import of including pregnancy and BIPOC status in examination of poor clinical outcomes. UMN found, in an analysis of 41,000 patient records, that both pregnancy and BIPOC status, after accounting for other covariates, were independently associated with poor clinical outcomes from COVID-19 infection….
The FDA has acknowledged that in addition to certain underlying health conditions, race and ethnicity “may also place individual patients at high risk for progression to severe COVID-19.” FDA’s acknowledgment means that race and ethnicity alone, apart from other underlying health conditions, may be considered in determining eligibility for mAbs. It is ethically appropriate to consider race and ethnicity in mAb eligibility decisions when data show elevated risk of poor COVID-19 outcomes for Black, Indigenous and other people of color (BIPOC populations), and that this risk cannot be adequately addressed by determining eligibility based on underlying health conditions (perhaps due to underdiagnosis of health conditions that elevate risk of poor COVID-19 outcomes in these populations). At the present time, MDH has found that available data show this elevated risk. While health systems should thus consider the elevated risks of progression to severe COVID-19 associated with race and ethnicity when making decisions about whether individual patients are eligible for mAbs, it is always the case that health care providers “should consider the benefit-risk for an individual patient.”
As I noted in my post about the New York COVID race discrimination scheme, this is unconstitutional: Use of race as a proxy for supposed greater risk—instead of focusing on the more directly relevant factors (“race-neutral alternatives,” in doctrinal terms), such as underlying medical conditions, vaccination status, lack of access to good alternative care, or the like—would violate the Equal Protection Clause in this situation. For instance, if the Department is concerned about underdiagnosis of health conditions, it could certainly provide funds to make sure that eligible patients are properly diagnosed; but it can’t just use being non-white or Hispanic as a stand-in for such supposed underdiagnosis. To quote Judge Amul Thapar in Vitolo v. Guzman (6th Cir. 2021), which rejected race-preferential COVID release funding,
The stark realities of the Small Business Administration’s racial gerrymandering are inescapable. Imagine two childhood friends—one Indian, one Afghan. Both own restaurants, and both have suffered devastating losses during the pandemic. If both apply to the Restaurant Revitalization Fund, the Indian applicant will presumptively receive priority consideration over his Afghan friend. Why? Because of his ethnic heritage. It is indeed “a sordid business” to divide “us up by race.” And the government’s attempt to do so here violates the Constitution.
This logic would apply even more clearly, I think, when the government explicitly discriminates based on race and ethnicity not just in funding but in access to potentially lifesaving drugs.
To be sure, the Court has left open the possibility that in some extraordinary emergency situation, where it is genuinely impossible to use a proxy, race or ethnicity can be considered, perhaps even in medical care. But there seems to be very little reason to think this is so here, especially given how heterogeneous the “BIPOC” group is; for instance, the Department cites this FDA document as support for its anti-non-BIPOC discrimination, and it in turn indirectly relies (through one of its few references that mentions race) on this CDC document (Obesity, Race/Ethnicity, and COVID-19):
Obesity Worsens Outcomes from COVID-19 …
Obesity Disproportionately Impacts Some Racial and Ethnic Minority Groups
Combined data from 2018-2020 show notable racial and ethnic disparities:
Non-Hispanic Black adults had the highest prevalence of self-reported obesity (40.7%), followed by Hispanic adults (35.2%), non-Hispanic White adults (30.3%), and non-Hispanic Asian adults (11.6%).
Hard to see how there would be any reason to think that “BIPOC” status as such—combining blacks, Hispanics, Asians, and American Indians of all backgrounds and economic status—is going to offer a consistent picture of any otherwise unmeasurable variables. Rather, “BIPOC” status is simply a distinction between those groups that this Minnesota government department chooses to prefer and those groups to whom it wants to be “deprioritizing access.”
Thanks to Hans Bader and to John Hinderaker (PowerLine) for the pointer.
The post Minnesota Government: "Deprioritiz[e] Access for Patients" to COVID Drugs, Based Partly on Their Being White appeared first on Reason.com.
from Latest – Reason.com https://ift.tt/31p0Z6M
via IFTTT