“America has a life expectancy crisis,” asserted a recent headline in The Washington Post. Why a crisis? Because American average life expectancy has been flat and then declining for the past decade or so.
One bit of recent good news: The Centers for Disease Control and Prevention (CDC) reported in November that average life expectancy at birth in 2022 was 77.5 years. While that is down from its 2014 peak of 78.8 years, the CDC notes that this is a post-pandemic increase of 1.1 years from its nadir of 76.1 years in 2021. The increase from 2021 to 2022, according to the CDC, “primarily resulted from decreases in mortality due to COVID-19, heart disease, unintentional injuries, cancer, and homicide. Declines in COVID-19 mortality accounted for approximately 84% of the increase in life expectancy.” While the big recent dip in American life expectancy was largely the result of the ravages of the COVID pandemic, the trend over the prior 10 years was basically flat.
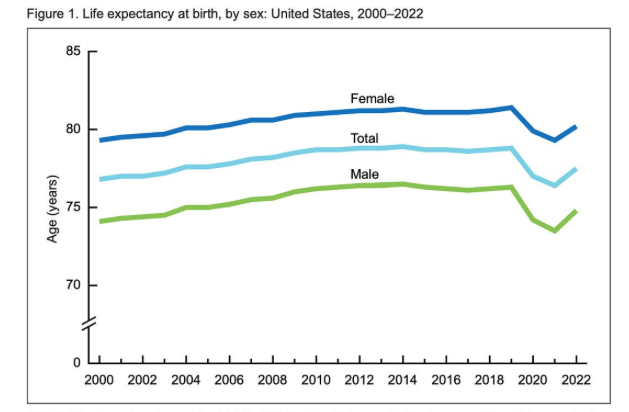
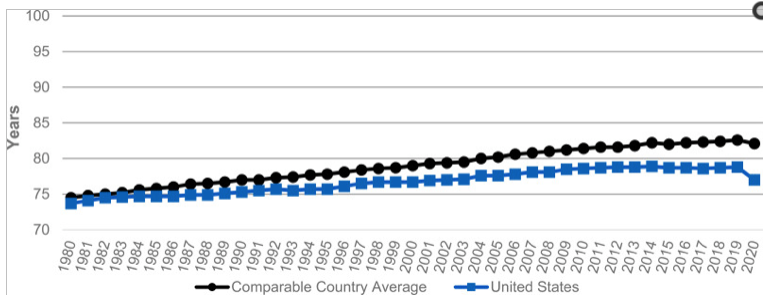
The Post article correctly noted that “the United States [was] increasingly falling behind other nations well before the pandemic.”
The Post asked numerous members of Congress, including all 100 Senators, what they thought about falling life expectancy. While many replied that it was a serious problem, the article concluded that it “is not a political priority.” The Post did acknowledge that “there also is no single strategy to turn it around.” Politics being the art of the possible, there is little that politicians can do at this point in biomedical history to significantly increase average life expectancy.
Public health efforts beginning the the late 19th century to provide access to clean water and improved sanitation, improve food safety, and champion widespread vaccination against infectious microbes were chiefly responsible for the increase in average American life expectancy from just 47 years in 1900 to the mid-70s in that late 20th century. “In 1900, one in 40 Americans died annually. By 2013, that rate was roughly one in 140, a cumulative improvement of more than two thirds,” reported a 2016 analysis by University of Pennsylvania researchers.
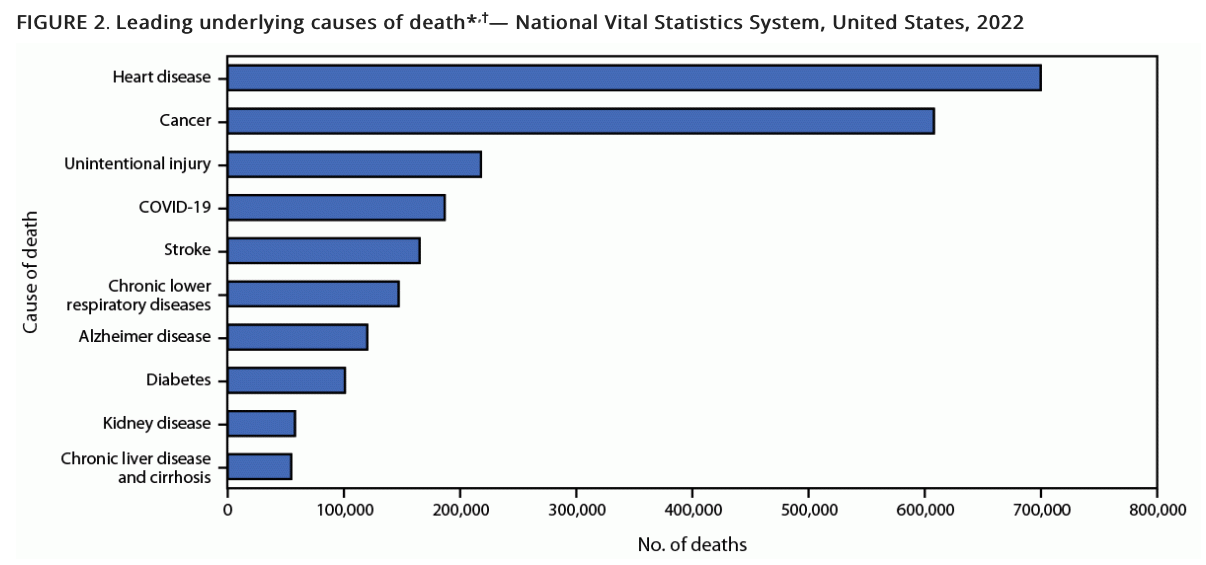
Today the leading causes of the deaths that mainly afflict older Americans are cardiovascular diseases, cancers, unintentional injuries, lower respiratory illnesses, and diabetes. Nostrums prescribed by politicians are not likely to have much effect on them.
Among other policies, the Post reported that many of the public health officials and lawmakers with which it spoke decried, “a health-care payment system that does not reward preventive care.” And why not? After all, an ounce of prevention is worth a pound of cure, right? Not necessarily, according to a comprehensive analysis of preventive care studies published in the Journal of the American Medical Association (JAMA) in 2021. “General health checks were not associated with reduced mortality or cardiovascular events,” noted the researchers. This bolstered the findings of a similar analysis in 2019 by researchers associated with the non-profit medical evidence review collaborative Cochrane that concluded that “health checks have little or no effect on total mortality.”
The Post article also suggested that fighting between congressional Democrats and Republicans has stymied “legislation linked to gains in life expectancy, including efforts to expand access to health coverage and curb access to guns.” As it turns out, various studies over the past two decades have calculated that lack of health insurance is associated with only a slightly higher risk of death.
A 2009 study in the American Journal of Public Health reported estimates that the lack of health insurance among Americans ages 25 to 65 may have been responsible for between 18,000 and 45,000 (0.8 to 1.8 percent) of deaths annually. At the time, 46 million Americans under the age of 65 were uninsured; by 2023 that had dropped to 23 million. As health insurance coverage increased, U.S. life expectancy stagnated and then fell.
What about guns? Unfortunately, the trends in both the rate and absolute number of firearm deaths—homicides, suicides, and accidents—have been upward over the past decade. The rate of firearm deaths hovered around 15 per 100,000 during the 1970s and 1980s and began to fall in the mid-1990s, reaching its lowest point at 10 per 100,000 in 2004.
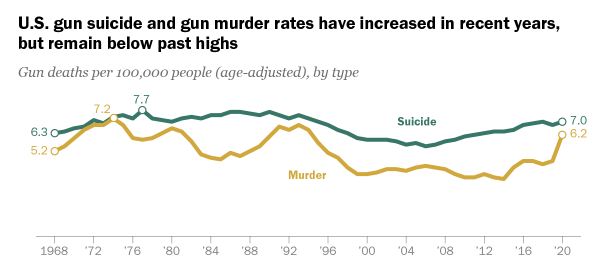
The rate of firearm mortality in the U.S. remained slightly over 10 per 100,000 over the next decade when in 2014 it began to rise, hitting in 2021 14.6 per 100,000, a rate last seen in the bad old days of the 1970s, 1980s, and 1990s.
Deaths from suicide have consistently been greater than those from homicide. In 2022, for example, the number of people who killed themselves using firearms reached 26,993 whereas those killed by others numbered 19,592. Most gun deaths occur at earlier ages, thus proportionately lowering the U.S. population’s overall life expectancy. A 2018 study in BMJ Evidence-Based Medicine calculated that firearm deaths between 2000 and 2016 reduced U.S. average life expectancy by 2.48 years. The researchers argued that other health gains during that period masked this countervailing downward life expectancy trend. And it does coincide with the slow-down in life expectancy increase that began around 2010.
What could politicians do about this? Setting aside constitutional issues, a 2023 comprehensive analysis of various policies aiming to reduce gun violence by researchers at the RAND Corporation think tank found relatively weak evidence that any of them worked all that well. For example, with respect to reducing violent crime, the evidence for the efficacy of policies such as banning assault weapons, imposing firearm safety training requirements, and requiring licenses and permits was inconclusive. Supportive evidence did, however, suggest that child access prevention laws could reduce youth suicides, accidents, and some violent crime deaths; and limits on concealed carry and stand-your-ground laws might reduce violent crime deaths.
The Post reported that some politicians pointed to the rising death toll from “lethal drug overdoses” as a significant factor in declining U.S. life expectancy. The Post did, however, acknowledge that drug deaths “are not solely responsible for the decline in life expectancy.” It is worth noting that opioid overdose deaths began truly soaring after 2010 when users turned to illicit heroin and fentanyl after the introduction of Food and Drug Administration–approved abuse-deterrent formulations.
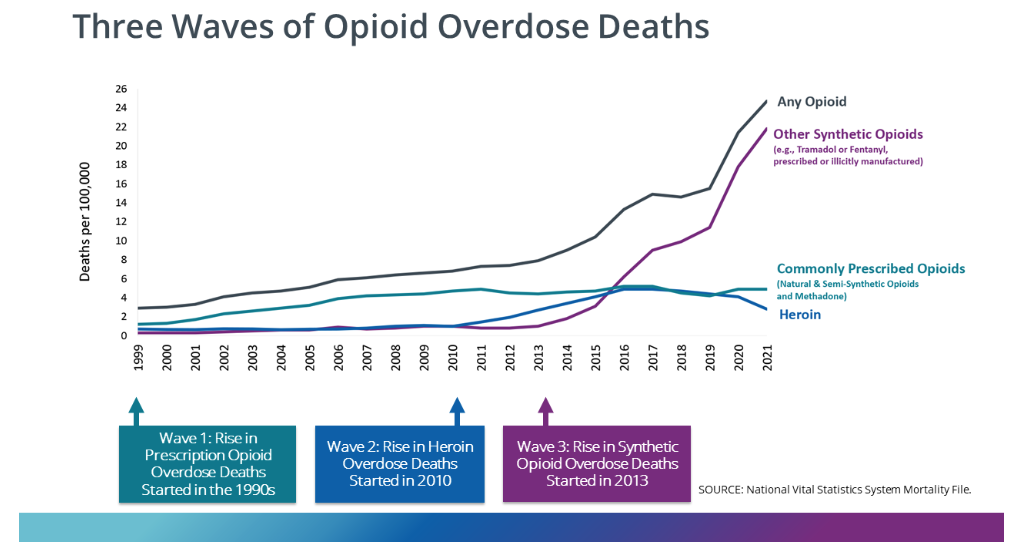
So how much do drug overdose deaths contribute to the recent decline in U.S. life expectancy? A 2021 comprehensive review of factors affecting mortality trends in the U.S. between 1999 and 2018 found that average life expectancy would “have been 0.3 years greater were it not for increases in unintentional drug poisoning.” In a 2023 preprint article, two Johns Hopkins University researchers calculated that opioid overdose deaths between 2019 and 2021 reduced U.S. life expectancy by 0.65 years. If politicians and policy makers really want to make increasing life expectancy a priority, one huge step would be to actually end the war on drugs. A cease-fire in the drug war would likely reduce gun deaths too.
The fact that Americans have been getting fatter has also contributed to the recent stalling of and then decline in U.S. life expectancy. A 2022 preprint by researchers associated with Oxford University and the University of Texas Austin calculates that properly accounted mortality from obesity is perhaps cutting U.S. life expectancy by 1.7 years.
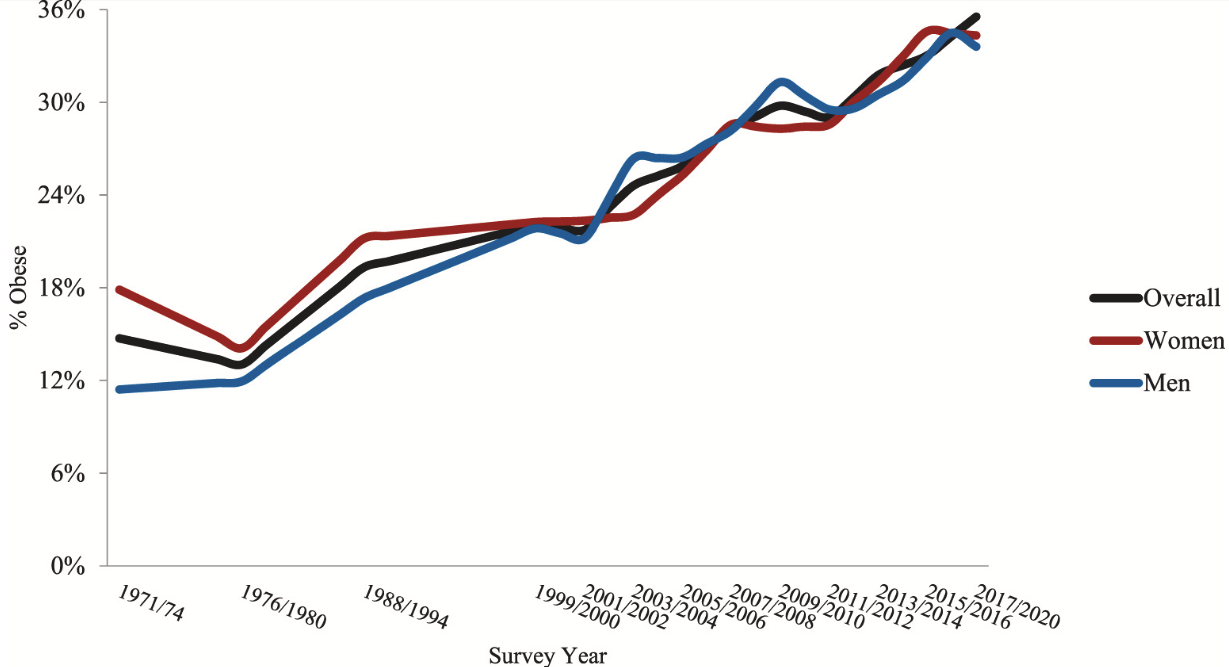
In a 2023 working paper, Socio-Behavioral Factors Contributing to Recent Mortality Trends in the United States, a team of demographers observed with considerable understatement that “hundreds of factors affect levels of mortality in every population.” They nevertheless gamely sought to identify possible factors for the changes in U.S. adult mortality over the period 1997–2019, using data from the National Health Interview Surveys (NHIS) for years 1997–2018. The variables they examined included alcohol consumption, cigarette smoking, health insurance coverage, educational attainment, mental distress, obesity, and race/ethnicity.
Among other things, the authors, in line with earlier studies, concluded that “changes in health care coverage, as measured here, had a negligible effect” on U.S. life expectancy trends over the past two decades. The two biggest factors they identified as affecting U.S. life expectancy trends were that “mortality falls with rising educational attainment” while “increasing mental distress contributed to the stagnation of mortality improvement.” Between 1997 and 2019, the percentage of college graduates rose from 24 percent to 36 percent of the U.S. population age 25 and above. Research consistently shows that college graduates tend to be less obese, smoke less, and eat better. Rising mental distress among NHIS participants as measured using the K-6 scale, especially after 2008, correlated with increasing mortality rates.
The nine-year difference in adult life expectancy between those Americans who are college graduates and those who are not is particularly striking.
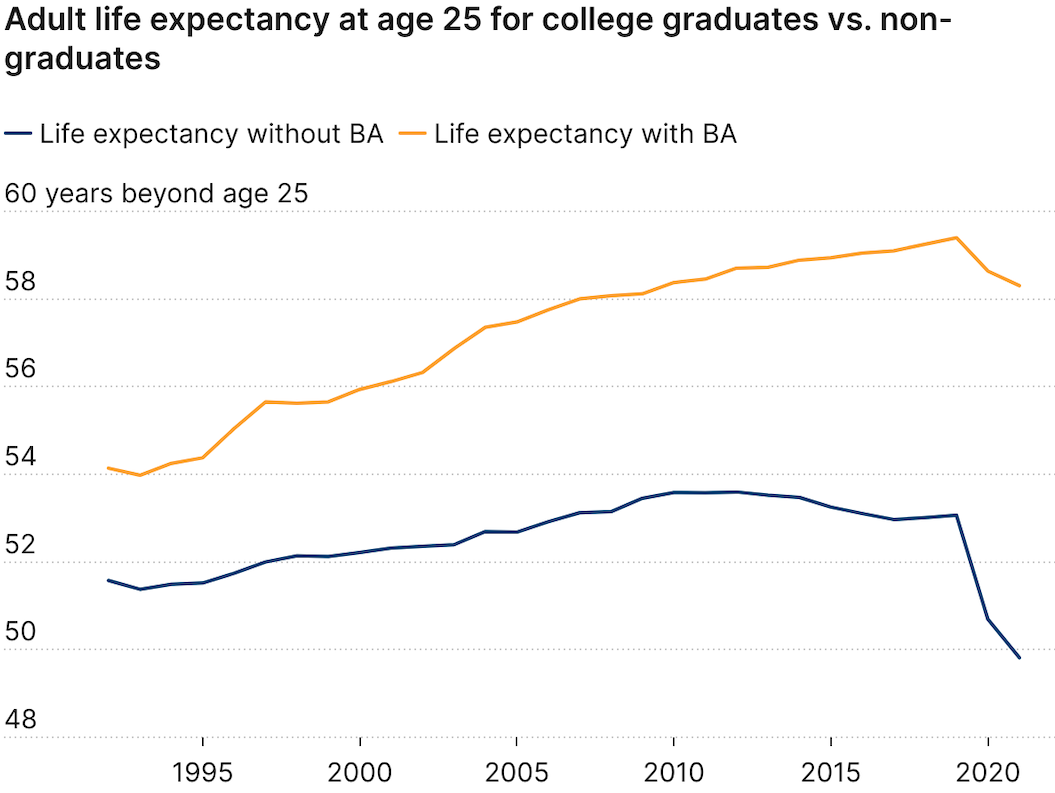
However, the U.S. is not alone with respect to differential socioeconomic life expectancy outcomes. Even countries famed for their government-run universal health care systems such as France experience them. For example, the European Commission’s 2019 country health profile of France reports that life expectancy for men and women in the top 5 percent of income is 84.4 and 88.3 years compared to those in the bottom 5 percent, which average 71.7 years and 80 years, respectively. This correspondingly results in male and female socioeconomic life expectancy gaps of 13 years and 8 years. The report notes that the gap in longevity can be explained at least partly by differences in education and living standards.
In the Post article, Sen. Bernie Sanders (I–Vt.) says that achieving Norway’s average life expectancy of 83 years should be our goal. It is worth noting that the life expectancy of adult American college graduates is 83.3 years, three years higher than the 80.3 years average for the relatively well-off countries that are members of the Organization for Economic Cooperation and Development.
A 2019 report from the Norwegian Institute of Public Health compared the average life expectancies of that country’s richest 1 percent with its poorest 1 percent. The report noted that “the differences in life expectancy between the one per cent richest and one per cent poorest in Norway were 14 years for men and 8 years for women.” A 2016 study in the JAMA reported essentially the same gap between America’s richest and poorest citizens. “The gap in life expectancy between the richest 1% and poorest 1% of individuals was 14.6 years for men and 10.1 years for women,” observed the researchers in JAMA.
“It has surprised researchers and policy makers that even with a largely tax-funded public health care system and relatively evenly distributed income, there are substantial differences in life expectancy by income in Norway,” said Dr. Jonas Minet Kinge, senior researcher at the Norwegian Institute of Public Health, in a press release about the report.
So why did U.S. life expectancy trends slow and then peak in 2014? And what, if anything, can policy makers and politicians realistically do to make increasing it a priority? As noted above, the big recent dip largely resulted from the COVID-19 pandemic. A 2023 Scientific Reports article “estimated that US life expectancy at birth dropped by 3.08 years due to the million COVID-19 deaths” between February 2020 and May 2022. But let’s set aside that steep post-2020 downtick in life expectancy resulting from nearly 1.2 million Americans dying of COVID-19 infections.
A 2020 study in Health Affairs chiefly attributed the 3.3-year increase in U.S. life expectancy between 1990 and 2015 to public health, better pharmaceuticals, and improvements in medical care. By public health, the authors meant such things as campaigns to reduce smoking, increase cancer screenings and seat belt usage, improve auto and traffic safety, and increase awareness of the danger of stomach sleep for infants. With respect to pharmaceuticals, they cited the significant reduction in cardiovascular diseases that resulted from the introduction of effective drugs to lower cholesterol and blood pressure.
So a big part of what propelled increases in U.S. life expectancy is the fact that the percentage of Americans who smoke has fallen from 43 percent in the 1970s to 16 percent now. Smoking is associated with higher risks of cardiovascular diseases and cancers, rates of which have been dropping for decades. In addition, the rising percentage of Americans who are college graduates correlated with increasing life expectancy.
However, since the 2004 peak, countervailing increases in the death rates from drug overdoses, firearms, traffic accidents, and diseases associated with obesity contributed to the flattening of U.S. life expectancy trends.
A 2021 comprehensive analysis of the recent stagnation and decline in U.S. life expectancy in the Annual Review of Public Health (ARPH) largely concurs, finding that “the proximate causes of the decline are increases in opioid overdose deaths, suicide, homicide, and Alzheimer’s disease.” Interestingly, the U.S. trend in Alzheimer’s disease prevalence has been downward since 2011. In addition, the ARPH review noted that “a slowdown in the long-term decline in mortality from cardiovascular diseases has also prevented life expectancy from improving further.” So enabling and persuading more properly diagnosed Americans to take blood pressure and cholesterol-lowering medications would likely boost overall life expectancy.
Hectoring members of Congress to make increasing life expectancy a “political priority” does not change the fact that there simply are no “silver bullet” policies available for achieving that goal.
The post Guns, Germs, and Drugs Are Largely Responsible for the Decline in U.S. Life Expectancy appeared first on Reason.com.
from Latest https://ift.tt/VkXlU2w
via IFTTT