Cascend: COVID Mortality Of A 74-Year-Old Man Is 2.68%
Tyler Durden
Fri, 10/02/2020 – 11:57
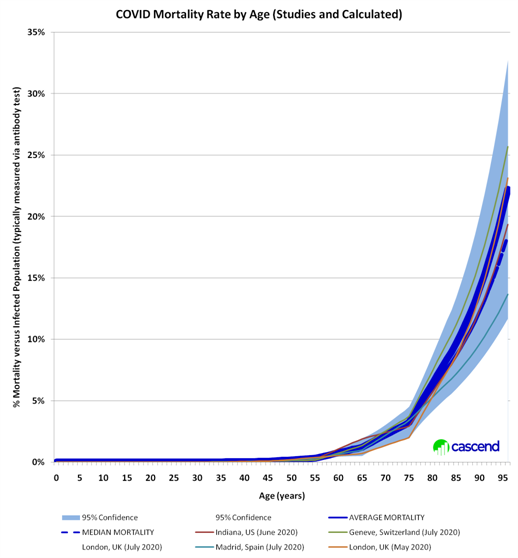
Now that Trump has admitted to having contracted the coronavirus, the next obvious – if morbid- question shifts to what are Trump’s odds of successfully emerging on the other side. To answer that question, Cascend Strategy calculates this morning that the Covid mortality rate for a 74 year old man – such as Trump – is 2.68%, or roughly 1 in 37.
Here are the details behind the Cascend calculation:
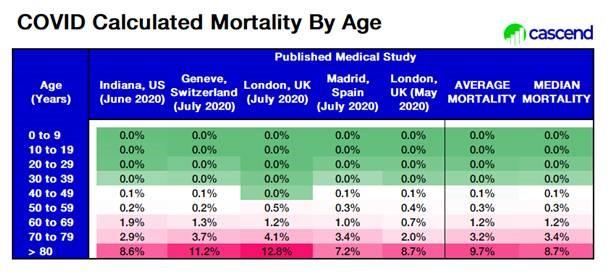
- The data is based on analysis of five recently published medical studies (May through July 2020; listed below) from U.S. and Europe.
- A study published in March from China likely vastly underrepresented the number of infections (denominator) and thus likely vastly overstates COVID mortality (8.6% for people in their 70’s)
- Males have roughly 19% higher mortality than average at that age (females have lower than average mortality)
- This assumes the population has no preexisting conditions: additional conditions add to the mortality rate
- President Trump is a 74-year old man with no known pre-existing conditions
- There are likely also inaccuracies caused by calculating mortality rates using infections measured with antibody tests: we discuss below how this may make mortality rates appear higher (smaller denominator) – actual mortalities may be lower, especially for populations who exhibit few or no symptoms
Cascend re-weighted studies by age to directly compare results
Some other observations from Cascend:
Doctors have noted President Trump’s weight as a factor
- However, we don’t have data of mortality versus weight (or BMI) to use for our analysis
- The studies we have found do not specify weight or BMI in their results
- So our data should only be corrected IF President Trump is substantially overweight (higher BMI) than the participants of these medical studies
- Common impactful pre-existing conditions include heavy smoking, diabetes, and heart disease
- Socioeconomic factors appear to have some impact on mortality rate
- There are also dispersions indicated by race/ethnicity, but it is unclear if these may be corrected by socioeconomic factors, or if there are other systemic factors
A study published in March from China (and heavily quoted by the Media today) likely vastly overstated mortality
- Data is significantly outside of the 95% confidence interval of the five other studies
- It likely underrepresented the number of infections (denominator) in our opinion
- And thus likely vastly overstates COVID mortality (8.6% for people in their 70’s)
- Data coming from China (particularly infections, mortalities and origin) has been questionable
- However China has been aggressive in administering quarantines, particularly at the beginning
- And this may instead be indicative of healthcare efficacy for older patients in China
Using Antibody tests as a measure of infections is a nice idea
- But it is likely systematically (and inadvertently) undercounting infections
- The newest most accurate antibody tests have 80% accuracy (based on a study from the University of Texas at Austin in collaboration with Houston Methodist study from two weeks ago) – on patients who have or just had COVID within the month
- However, this is measuring antibodies for patients that have COVID or just had it – high viral load
- Antibody tests on patients who had COVID but waited several months cause accuracy to be much lower
- CDC Director Robert Redfield said in June that true case numbers are 10 times higher than confirmed diagnoses.
- (Confirmed cases in the U.S. were 3.8 million at the time– that means 38 million U.S. infections likely)
* * *
Works cited:
1) Indiana University (Richard M. Fairbanks School of Public Health) and the Indiana University School of Medicine (Justin Blackburn, PhD, Constantin T. Yiannoutsos, PhD, Aaron E. Carroll, MD, MS, Paul K. Halverson, DrPH, Nir Menachemi, PhD, MPH)
2) “Serology-informed estimates of SARS-CoV-2 infection fatality risk in Geneva, Switzerland Javier Perez-Saez, Stephen A Lauer, Laurent Kaiser, Simon Regard, Elisabeth Delaporte, Idris Guessous, et al.; Published:July 14, 2020; DOI:https://doi.org/10.1016/S1473-3099(20)30584-3
3) “Antibody prevalence for SARS-CoV-2 in England following first peak of the pandemic: REACT2 study in 100,000 adults; Ward, Christina J Atchison, Matthew Whitaker, Kylie E. C. Ainslie, Joshua Elliott, Lucy C Okell, Rozlyn Redd, Deborah Ashby, Christl A. Donnelly, Wendy Barclay, Ara Darzi, Graham Cooke, Steven Riley, Paul Elliott; doi: https://doi.org/10.1101/2020.08.12.20173690
4) “Infection fatality risk for SARS-CoV-2: a nationwide seroepidemiological study in the non-institutionalized population of Spain
Roberto Pastor-Barriuso, Beatriz Perez-Gomez, Miguel A Hernan, Mayte Perez-Olmeda, Raquel Yotti, Jesus Oteo, Jose Luis Sanmartin, Inmaculada Leon-Gomez, Aurora Fernandez-Garcia, Pablo Fernandez-Navarro, Israel Cruz, Mariano Martin, Concepcion Delgado-Sanz, Nerea Fernandez de Larrea, Jose Leon Paniagua, Juan Fernando Munoz-Montalvo, Faustino Blanco, Amparo Larrauri, Marina Pollan, Marina Pollan; doi: https://doi.org/10.1101/2020.08.06.20169722
5) “Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study Amitava Banerjee, DPhil Laura Pasea, PhD Steve Harris, PhD Arturo Gonzalez-Izquierdo, PhD Ana Torralbo, PhD Laura Shallcross, PhD et al.; Open AccessPublished:May 12, 2020DOI:https://doi.org/10.1016/S0140-6736(20)30854-0
6) Estimates of the severity of coronavirus disease 2019: a model-based analysis (data from Wuhan); Robert Verity, PhD; Lucy C Okell, PhD; Ilaria Dorigatti, PhD; Peter Winskill, PhD; Charles Whittaker, MSc; Natsuko Imai, PhD et al. Published:March 30, 2020
via ZeroHedge News https://ift.tt/2EXQUm2 Tyler Durden